 loading
loading
Old YalePioneers in chemotherapyJudith Ann Schiff is chief research archivist at the Yale University Library.
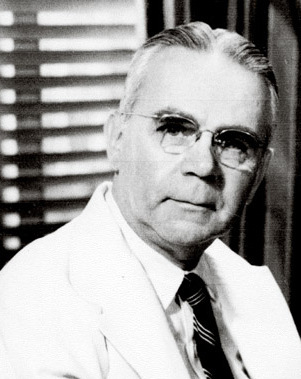 Harvey Cushing/John Hay Whitney Medical LibraryThoracic surgeon Gustaf Lindskog worked with two pharmacologists to provide a dying cancer patient with an experimental therapy. View full image
It was at Yale that intravenous chemotherapy, now an invaluable part of cancer treatment, was first administered to a cancer patient and shown to have a powerful effect on human tumors. Sadly, in this first-ever trial, the treatment was not yet advanced enough to save the patient’s life. Alo sadly, he cannot be memorialized for his part in the trial; privacy laws prohibit the release of his name, even decades after his death. But three Yale School of Medicine doctors have recently discovered his long-lost medical records. In a recently published article in the Journal of the American College of Surgeons, Yale medical professors John E. Fenn and Robert Udelsman recount their efforts to track down the records, which were finally found in the files of the Yale Department of Pathology through a search led by Michael Kashgarian, professor emeritus of pathology. Thanks to their work, this landmark course of treatment can now be known. Yale’s chemotherapy work came about as a result of the development of chemical warfare—specifically mustard gas, first used by the Germans on the Allies in World War I, with devastating results. During World War II, medical school dean Milton C. Winternitz arranged a government contract to investigate new chemical warfare agents. In 1942, he assigned two research pharmacologists to study nitrogen mustard compounds, newly developed relatives of mustard gas. The two were Alfred Gilman (1908–84) ’28S, ’31PhD, and Louis S. Goodman (1906–2000), a graduate of the Johns Hopkins medical school. Both were assistant professors of pharmacology and toxicology, and together they wrote what became the standard textbook in the field. The project was so secret that, in their notes, Gilman and Goodman referred to the nitrogen mustard compound they used as “X.” In seeking ways to counteract X’s toxicity, they noticed that it killed lymph and white blood cells in rabbits—suggesting that it might work on malignant tumors. They obtained a mouse with a large tumor from a colleague and treated it successfully, although the tumor returned. A second treatment produced less decrease in the tumor, and the third none at all. But the treatment greatly prolonged the mouse’s life. The two presented their data on treating mouse lymphoma to Gustaf E. Lindskog, a thoracic surgeon who was then a professor of surgery. In August 1942, Gilman and Goodman would treat their first chemotherapy patient, in Lindskog’s clinic. “JD” was an unmarried 47-year-old Polish immigrant who had worked in a Connecticut ball bearing factory. He had been in pain for some months before he came to the clinic, where he was first treated in January 1941 for lymphosarcoma in his neck and cervical region. Multiple radiation treatments were at first successful but by the end of the year had no effect, and he was in great distress. Notes entered in the medical record on August 25, 1942, read: “The patient’s outlook is utterly hopeless on the present regimen. Because the end seems near he should be in the hospital. Dr. Lindskog will investigate the possibility of obtaining one of the newer chemicals which are lymphocidal. Immediate admission arranged.” JD consented to the treatment, at any risk. On August 27, at 10 a.m., the first of ten daily doses of chemotherapy was given. “Judging how much ‘synthetic lymphocidal chemical’ [to use] can be tricky,” reads a note in the record. There was no precedent for the dosage, but Gilman and Goodman extrapolated from their rabbit studies. Four days later the patient said he could sleep, eat, and move better. By September 6 he had greatly improved. But his white blood cell and lymphocyte counts began to fall. With blood transfusions to treat the falling blood cell counts, JD continued to improve. On September 27, “all cervical and axillary nodes [of the cancer] were gone.” But by mid-October his lymphosarcoma was back. The second cycle of dosage had only short-term effectiveness, showing that the cancer cells were beginning to develop resistance. (To combat this problem, chemotherapy now combines several different compounds.) The third and final six-day dosage was started on November 6. It had little effect. JD’s tumors continued to grow, and he died on December 1, his 96th day in the hospital. Nitrogen mustards are still among the most widely used chemotherapy agents today. In their article, Fenn and Udelsman credit Lindskog, who “had a special oversight and intense interest in JD’s management,” with an important role in Yale’s work to use them against cancer: “Without Lindskog’s initiative, this first use of an intravenous chemotherapeutic agent would not have taken place.” The surgeon continued teaching at Yale until 1971 and was widely recognized for his work in thoracic surgery. Gilman and Goodman both left Yale in 1943. Goodman had a distinguished career as a pharmacology professor at the University of Vermont and the University of Utah. Gilman became a professor at Columbia University; later, he helped establish the Albert Einstein College of Medicine. He returned to Yale in 1973 as a lecturer in pharmacology, continuing until his death in 1984. In the Class of 1928 reunion milestone histories, Gilman made no mention of his historic achievement, stating simply, in 1958: “The life of teaching and research in academic medicine has been most satisfying.”
The comment period has expired.
|
|